Jeremy Nobel of the Center for Primary Care at Harvard Medical School where he teaches a course on loneliness and public health says “The experience of loneliness is 100 percent subjective. Isolation is the objective state of being physically separate. Loneliness is the self-perceived gap between our social connectedness and that which we aspire to have.”
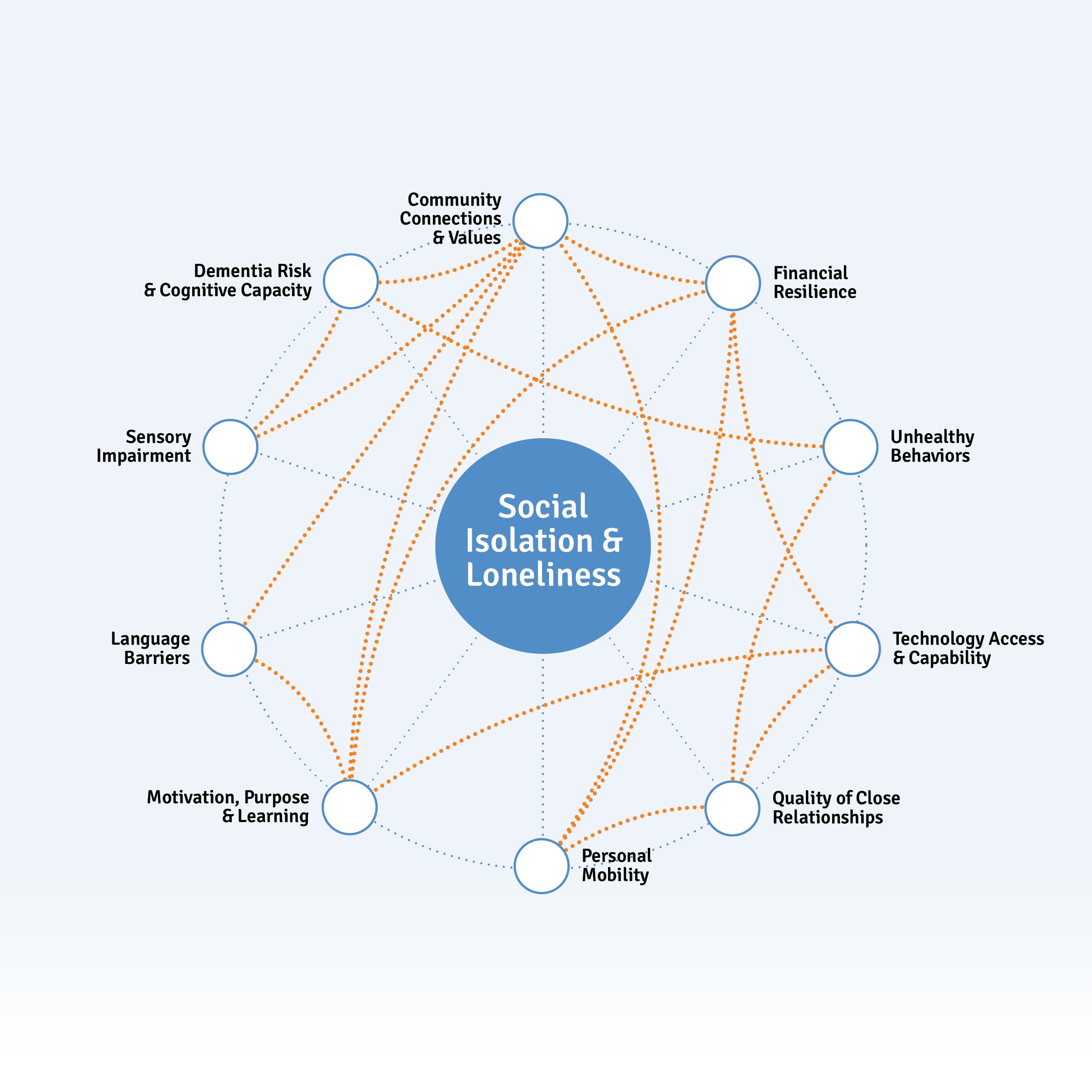
Interconnected Issues for Social Isolation & Loneliness
Many interrelated factors are noted here, and can be grouped into several subcategories which are expanded upon below:
- Impact on Health
- Financial Resilience
- Community Connections & Values
- Caregiving
- Community-Based Support
- Personal Capacity
Impact on Health
Social isolation and loneliness increase a person's risk of mortality. They have been linked to a greater risk of heart attack, metastatic cancer, stroke, depression, dementia and neurodegenerative diseases. Research from UCLA shows that lonely adults are 25% more likely to die prematurely. Elderly people who are lonely die at twice the rate as those who are socially connected. All of which makes the spike in loneliness in American society even more alarming.
Older people who are socially isolated are more likely to have less healthy behaviors, like poor diets, tobacco use and lack of physical activity. Socially isolated individuals have an increased risk of developing depression, anxiety and dementia. They are also more vulnerable to abuse - both financial and physical. Social isolation can also make the client more susceptible to elder financial abuse as perpetrators of such crimes can more easily take advantage of the isolated elderly.
A seminal work on the medical effects of loneliness in 2010 showed that:
- Loneliness, living alone and poor social connections are as bad for your health as smoking 15 cigarettes a day.
- Loneliness is worse for you than obesity.
- Loneliness is likely to increase your risk of death by 29%
One of the earliest, and longest studies on Social Isolation and Loneliness is from the multi-generational, Framingham Heart Study (begun 1948) found that lonely people are less able to pick up on positive social stimuli, like others’ attention and commitment signals, so they withdraw prematurely – in many cases before they’re actually socially isolated. Their inexplicable withdrawal may, in turn, make their close connections feel lonely too. Lonely people also tend to act “in a less trusting and more hostile fashion,” which may further sever social ties and impart loneliness in others.
The report also observed what it describes as the contagion of loneliness which can be found in six groups:
- Family-related loneliness
- Disability and aging
- Resource-constrained groups
- Stigmatized groups
- Occupational loneliness
- Deliberately isolated groups.
Financial Resilience
The AARP estimates that prior to the pandemic, poor social relationships were associated with a 29% increase in risk of coronary heart disease and a 32% rise in the risk of stroke, and in 2017, $6.7 billion was spent in federal funding to assist social isolation among older adults.
Senior loneliness is an epidemic in the United States and globally. It is of such seriousness that in 2018, the UK created the position of the Minister for Loneliness.
Some healthcare programs have been introduced in the US to help seniors at risk of loneliness. One initiative at CareMore enrolled 1,000 clients, who, over the period of the trial, patients became less lonely and used fewer healthcare resources. “Enrollees decreased their emergency department (ED) utilization by 3% in year one, while a comparison group increased ED use by more than 20%. Hospital admissions among program participants are 21% lower than among the comparison group.”
Community Connections & Values
With the advent of the contraceptive pill in the 1960's, Baby Boomers became the first generation to choose whether or not they wanted to have children, or how many they might have. This is having a significant impact on their aging, as many are now childless and unmarried, and at risk of becoming ‘elder orphans’.
With 10,000 baby boomers turning 65 each day in America, childlessness is also growing. The U.S. Census data in 2012 showed that about one-third of Americans aged 45 to 63 were single - a 50% increase since 1980. In 2018, that figure was 15 million adults nationwide - 27% of adults aged 65+ are currently elder orphans in that they have no children to look after them as they age.
This presents a tremendous problem for older Americans, as adult children are the primary caregivers to most senior adults, with approximately 43.5 million caregivers having provided unpaid care in (2015) at an estimated economic value of $470 billion in (2013).
Prevalence of Social Isolation & Loneliness in Orange County
The American Community Survey (ACS 2019 table S1101) estimates that of the approximately 1,044,280 households in OC:
- 9.5% (or 99,207) are individuals aged 65+ who live alone
- 42.4% of all households in OC (442,385) have at least one person who is aged 60+
- 28.5% of all households in OC (297,117) are ‘non-family’ households
- 48.2% (~143,210) of ‘non-family’ households have at least one member who is 60+ years old
- Of the 297,117 non-family households, 33.6% are 65+ who live alone.
The most fulsome report on social isolation and loneliness in Orange County comes from the AARP Connect2Affect isolation map. This is based on the Orange County population aged 50+ and is modeled on small area estimates based on National Social Life, Health and Aging Project Survey (2015-2016) (NSHAP) data. The survey measures the self-reporting frequency as feeling (1) a lack of companionship, (2) left out, (3) isolated.
Throughout the report, you will see different terms for different estimates from ACS. For some factors they measure the number of households. For others they will count individuals. The Census surveys a different age range to the AARP survey.
According to OC Healthier Together, approximately 95,120 individuals or 20.9% of adults aged 65+ in OC lived alone in 2019.
The Connect2Affect map shows 20.7% of adults in Orange County aged 50 and over are at risk of loneliness through social isolation.
The ACS shows that 20% of Orange County is aged between 50<65 (637,397) (132,000 at risk of Social Isolation.) If you subtract the 50<65 age from the group.
The range of estimates of adults aged 65+ at risk of social isolation is between 95,000 and ~101,000 individuals in Orange County.
| Measures of Social Isolation | Orange County | California | United States |
|---|---|---|---|
| Loneliness Score (population 50 and older) | 1.2 | 1.2 | 1.1 |
| Percent of population 50 and older who attend religious services once a month or more | 37.80% | 37.80% | 44.80% |
| Percent of population 50 and older who participate in group activities once a month or more | 44.50% | 42.40% | 41.90% |
| Percent of population 50 and older who socialize once a month or more | 82.30% | 81.80% | 79.10% |
| Percent of population 50 and older who volunteer once a month or more | 27.60% | 26.20% | 28.50% |
| Percent of population 50 and older with high loneliness scores | 20.60% | 21.10% | 20.00% |
| Membership associations per 10,000 | 5.9 | 5.9 | 9.3 |
| Social Engagement Composite Score (population 50 and older) | 8.9 | 8.8 | 9.1 |
| Social Engagement Domain Score (population 50 and older) | 1.9 | 1.8 | 1.9 |
| Risk of Social Isolation (population 65 and older) | 20.70% | 29.10% | 0.00% |
Several surveys, including the 2018 Orange County Needs and Gap Analysis Report, asked respondents about their experiences with social isolation. These data sources are valuable because they allow for a deeper understanding of how other concerns may be related to it. The Orange County Aging Services Collaborative 2018 OC Senior Living Needs survey includes a variety of crucial information on seniors including lifestyle, socialization, finances, counseling, transportation, and connection.
From these reports we can see that in 2019, 93,120 adults in Orange County, aged 65 and over, lived alone. And in March 2021, the Conduent Healthy Communities Institute reported that 24.4% of Orange County adults aged over 65 have difficulty speaking English. These are two separate facts which predispose an individual to isolation, potentially leaving them without sufficient access to health and wellness resources.
One direct measure of social connection (rather than isolation) among older adults is that approximately 11.3% (or 54,838) of adults 65+ in Orange County engage in volunteer work (CHIS 2015-16). What is unclear about this measure, is that we do not know if these older adults live alone or in family households, and whether they participate as couples or individually.
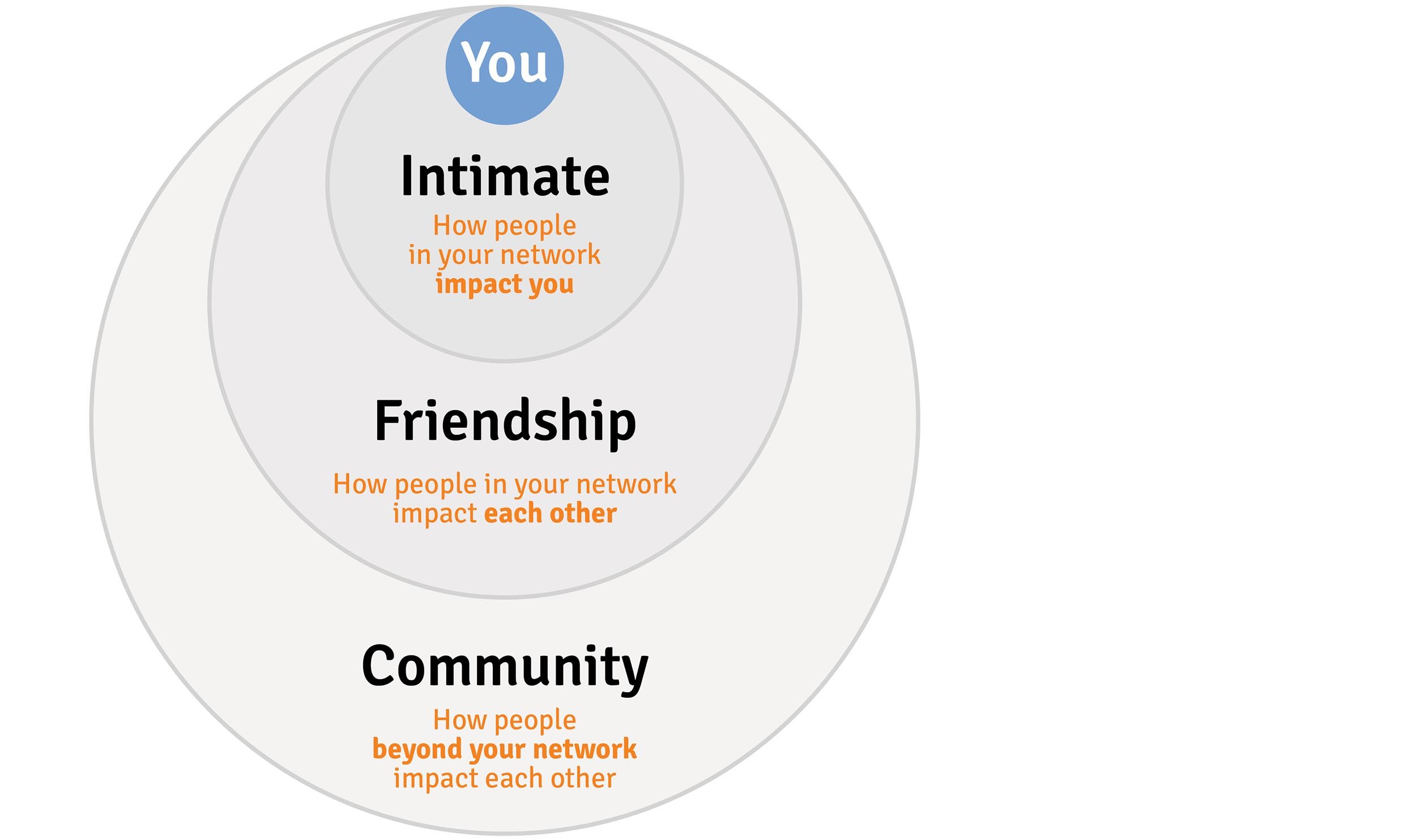
Social Networks
Among the interconnected issues which increase social connectedness for individuals are:
- Community Connections & Values
- Quality of Close Relationships
- Motivation & Purpose
In 2016 the Red Cross UK released a review of literature relating to isolation and loneliness which said that in general, women report feeling lonely more than men, but surveys which omit the word “lonely” generally find that men feel lonelier than women.
“A county’s Social Isolation Risk Score is a composite measure of six risk factors. These include whether residents live in poverty; live alone; are divorced, separated or widowed; never married; have a disability; and have difficulty with independent living.” Lisa Marsh Ryerson President AARP Foundation 2018
A University of Michigan & AARP study on isolation during Covid-19 found that feelings of isolation increased significantly between 2018 and 2020. Isolation was felt more significantly among females, lower income, lived alone, were unemployed or disabled, caregivers, and lower in mental or physical health.
Older people become isolated when their health makes it difficult to leave the house or their partners die. Feelings of loneliness increase if they become caregivers because their partners develop chronic health conditions, and the demands of caregiving lead them to feel very much alone. This affects:
- Retirees
- Widowed
- Recently retired
- Unable to meet friends family regularly
- Unable to interact with neighbors
- Poor health
- Suffering from depression
- Suffering from poor mobility
- Visually impaired
- Hard of hearing
- Struggling financially
- Veterans
The AARP Foundation and NORC at the University of Chicago have produced an interactive map called connect2affect to understand social isolation in America. It includes a short quiz based on the UCLA Loneliness Scale to gauge individual loneliness. The questions reflect these key metrics of Social Isolation & Loneliness:
- Time spent in group or social activities either virtually or in person.
- Regularity of conversations with family or friends
- Provision of frequent care for a friend or family member who needs you.
- Ease of access to transportation
- Ability to leave home without assistance
- Ability to hear in a group
- Feelings of isolation from others
- Major change or loss
“We find that people who are more connected are healthier and healthier people are more connected, it’s bi-directional. Research has shown that human connection is a big way we get through tough times. We don’t do nearly as well isolated as we do together.” Robert Waldinger, Prof Harvard Medical School
Imagine it like this hierarchy of Positive Relationships (can be built in both directions) Credit: Sheridan Jobbins and Erica Young
Being alone and lonely can result in a kind of emotional inertia which requires effort to reach out.
- Stay connected
- Daily effort to express gratitude
- Do something for others
- Collaborate harmoniously
- Volunteer
- Engage with others including strangers
- Share positive news
The AARP tells us: Fewer adults who belong to a local community felt lonely 26% - compared to 39% who did not. Volunteers who had volunteered in the past year were substantially less lonely (28 %) than the 40% who had not.
Caregiving
The one area of help where this is reversed is for caregivers who provide unpaid care for an adult friend or family member with an age, disability or health-related issue. Caregivers are more inclined to loneliness (42%) than other midlife or older adults (34%).
Community-Based Support
During the pandemic shutdowns, the City of Fullerton Senior Center staff reached out to their program participants, provided training on how to connect virtually, and expanded virtual programming in order to prevent increased isolation among its senior center participants.
Other senior-specific programming exists throughout the county through organizations like Osher Lifelong Learning Institute, and Saddleback College Emeritus Institute. Saddleback’s Emeritus Institute provides more than 200 classes at a variety of locations throughout the county, ultimately serving more than 6,000 older adults annually. This programming provides support for overcoming the digital divide, building friendships and social interaction, and continued intellectual development. The pandemic shutdowns have forced some of these programs to move to Zoom or other online tools which has mitigated some of their positive support, but the return to in-person programming will bring back these positive benefits.
A survey conducted by the University of Michigan in association with AARP indicated that interactions with neighbors mitigated much of the loneliness and isolation felt by older adults during the early months of the pandemic. But from March–June 2020, many older adults reported connecting with family or friends outside their home using social media (70%) and video chat (57%). Three in five (59%) used social media and 31% used video chat once a week or more. Yet adults aged 50–80 who used social media were more likely to report feeling isolated than those who did not use social media (58% vs. 51%). In this instance, the digital divide may have both mitigated and attenuated the impact of the pandemic shutdowns on social isolation among seniors.
SoulRapha in Tustin is one of the few community-based organizations that is mandated to relieve loneliness. Their main area of concern is that 60% of residents within assisted living facilities, do not have regular visitors. Figures from SoulRaph indicate that in Orange County California there are:
- 8,300 skilled nursing residents
- 14,350 assisted living residents
- 35,000 seniors enter and leave some form of assisted living care every year
The Council on Aging Southern California helps resolve problems and advocates for the rights of providing support to isolated long-term care residents through its Long-Term Care Ombudsmen program and other services.
Through the Orange County Strategic Plan for Aging, a number of community organizations have collaborated for several years to provide quarterly OC Heart to Heart Visitation Council meetings and an annual conference to bring together the many organizations that offer different types of friendly visitor programs. Participating organizations include Alzheimer’s Association – Orange County Chapter, Alzheimer’s Orange County, CalOptima, City of Costa Mesa, City of Fountain Valley, City of Westminster, Council on Aging – Southern California, Laguna Woods Village, OC Office on Aging, Project LIFE, Meals on Wheels OC, and St. Jude Medical Center.
During the pandemic, the California Department of Aging established a phone line to support older adults who were experiencing social isolation (CHHS data). The “friendship line” received 2680 calls from Orange County residents between April 13, 2020 and October 4, 2020. This is an average of 15.4 calls per day during that period (2680 calls / 174 days).
The 2021 OC Community Indicator report shows a declining trend of older adult hospitalizations for mental health disorders (p127).
One metric to consider when measuring isolation and loneliness is suicide. “Suicide in later life is a global public health problem, with those aged 65 and above constituting the demographic group with the highest suicide rate in most countries that report suicide statistics to the World Health Organization.”(WHO) The suicide rate of adults age 65+ in OC is approximately 15.8 per 100,000. “Men are about four times more likely than women to die of suicide, but three times more women than men report attempting suicide. Suicide occurs at a disproportionately higher rate among adults 75 years and older.”
There is a lot of academic literature about the relationship of social isolation, loneliness and suicide by older adults. One of the noted problems in measuring the impact of social connection, is the difficulties of engaging socially isolated populations at all. The conclusion from the first study into the problem (Improving Social Connections to Reduce Suicide Risk: A Promising Intervention Target) was that while more study is needed for reducing suicide itself, “Social Engagement was effective in reducing depressive symptoms and improving social-emotional quality of life.”
The intersection between mental health and older adult social isolation is even more complicated by language barriers or cultural biases. The UCI 2019 Health Needs Assessment has a list of mental health indicators from CHIS but they are not older-adult specific (p 53). “For our aging population, there are often cultural biases that regard mental health as a stigma. They get to a point where problems are escalating and reach a critical moment, when intervention is needed at a higher level of care”
2019 ACS data (Table S1601) show the disparity of impact that language barriers have on the older adult population in Orange county. For example, of the overall population of Spanish speakers in Orange County, 35.2% speak English ‘less than very well.’ However, when you take the subset of Spanish speakers who are aged 65+, the percentage who speak English ‘less than very well’ jumps to 65%. A staggering 77.9% of 65+ adults who speak API languages speak English less than very well.
Community Networks
Among the issues which increase social connectedness for individuals are:
- Personal Mobility
- Technology Access & Capability
- Age Friendly Neighborhoods
Adult day care services are a vital part of age-friendly neighborhoods. They provide opportunities for older adults to socialize and receive other support. The Orange County Office on Aging Service Unit Plan for 2020-24 has goals for a number of services that have a socialization component, including: in-home care, home delivered meals, adult day care, congregate meals, information and access, outreach, and senior center activities.
Cities throughout the county sponsor programs for older adults through their parks and recreation departments (e.g. art classes) and at senior centers.
- Garden Grove’s senior center served around 150 older adults (during the pandemic) with classes mostly revolving around physical activity. They are partnering with Santa Ana college for technology training in the spring.
- The City of Mission Viejo’s senior center served approximately 4,536 seniors (pre-pandemic) with a wide range of classes including many focused on technology.
- The City of Buena Park’s senior center had a pre-pandemic attendance of between 500-600 seniors. They have a 20 person computer lab with tutors available 5 days per week.
“I enjoy my visits with the Meals on Wheels driver. Bill is super-duper. He’ll talk to us for like five minutes. Sometimes he’s the only interaction with other people in the week.”
Healthcare provides an opportunity for older adults to be out and receive some social attention. The pandemic also shifted most of these visits to virtual appointments (telehealth) which increased social isolation among those already experiencing the digital divide.
"It would be nice to have someone just vusit us. ou know, shoot the breeze, do some handman work around the house, and just hang out for 30 mins."
The 2021 CalOptima report demonstrates the staggering growth of telehealth visits from the pandemic. During Q3 2020, CalOptima experienced 202,164 telehealth visits, 84,119 of which were behavioral health. (This data is not detailed by age group.)
Personal Capacity
In their study on Improving Social Connections to Reduce Suicide Risk, researchers observed that “Engaging the most socially isolated older adults in interventions poses a significant challenge.” Factors which influence older adults ability to connect with others around them include:
- Language Barriers
- Financial Resilience
- Sensory Impairment
- Faith or Spirituality
[The AARP tells us:](https://www.aarp.org/content/dam/aarp/research/surveys_statistics/life-leisure/2018/loneliness-social-connections-2018.doi.10.26419-2Fres.00246.001.pdf (Below)) Adults aged 45+ without spiritual or religious connections are more likely to be lonely (39%) than to those who identify as very religious or spiritual (25%).
Religious organizations provide opportunities for older adults to connect socially and receive support from one another. While overall religious engagement has declined, rates of religious participation among older adults has fallen least. Estimates of religious membership and participation are not disaggregated by age group) which makes it difficult to identify what portion of the older adult population is receiving support from them.
The Orange County Interfaith Network (OCIN) helps coordinate the work of various interfaith councils. At present there are 13 active interfaith councils throughout Orange County.
Anecdotally, religious congregations in Huntington Beach helped identify the food insecure and helped distribute significant amounts of support during the earliest days of the pandemic. Doing this, they identified some of the difficulties in reaching isolated individuals.
“People are in denial. They’re in denial about how bad their situation is getting and they’re afraid if they’re discovered they’ll lose their house or independence. They’ve been independent their entire lives and now they need help.”
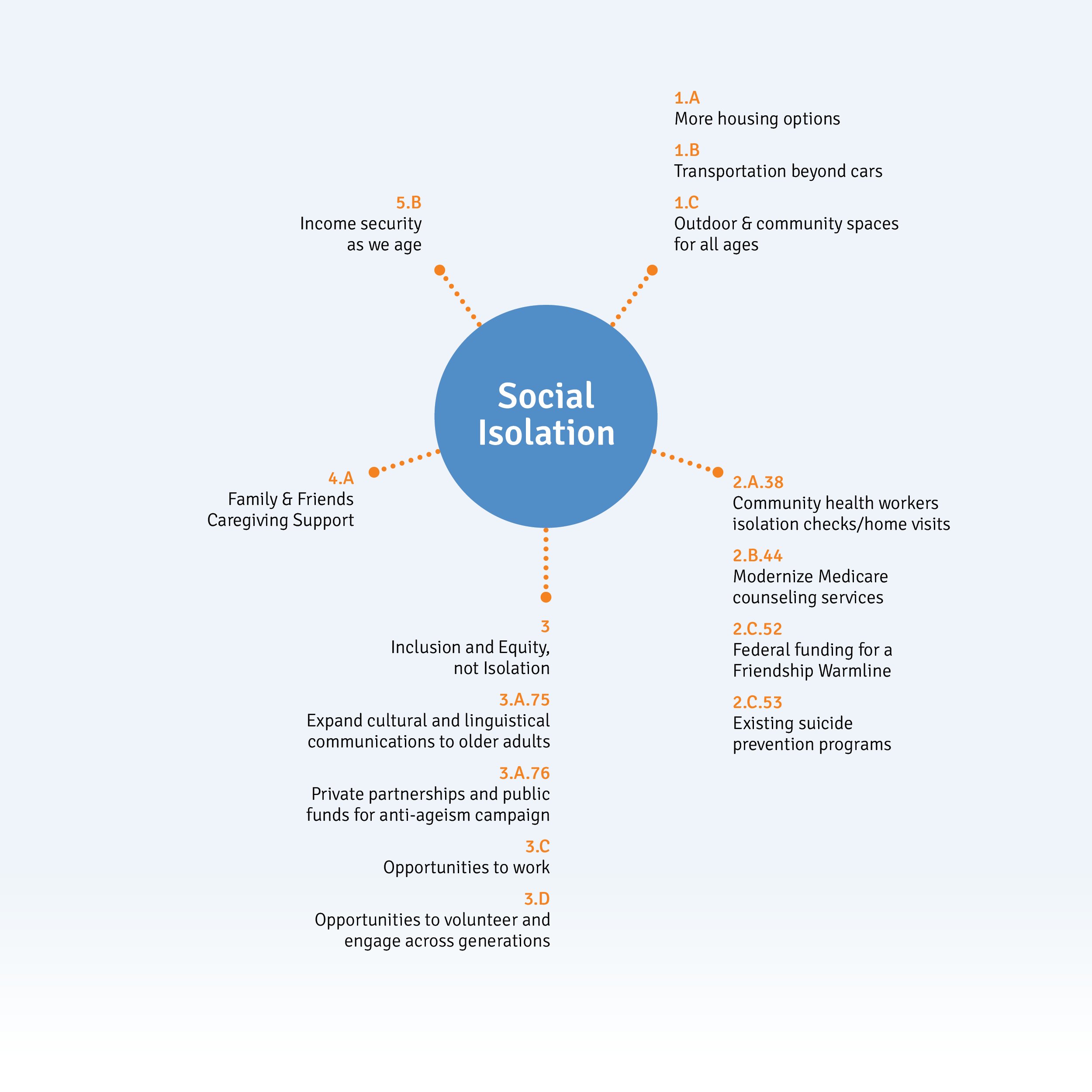
California’s Master Plan for Aging Initiatives Relating to Social Isolation & Loneliness
Reference numbers relate to California’s Master Plan for Aging’s Five Bold Goals for 2030 to be used with their progress dashboard and budget.
While the Master Plan for Aging explicitly targets social isolation only via isolation checks and friendship warm lines, it has many initiatives which target the underlying causes and effects. This includes the connectedness of family, friends, community and health services, as well as age-friendly transport to move between locations.
The impact of affordability, particularly as it relates to housing, features strongly in strategy 1A for More Housing Options. This not only highlights the need for more subsidized housing per 100,000 population but also that, “including Accessory Dwelling Units and Residential Care Facilities of all sizes, will support older adults, caregivers, and their families.” The identified need is cost-effective mixed dwelling housing, so people can live together and support each other to age in place.
Green spaces with a social dimension are described as something that “all Californians can benefit from” with the objective of “convenient park access within a ten-minute walk or less, co-location of parks with community centers offering programming for all ages”. While not explicitly about social isolation, this combines access to nature with exercise and places to congregate. Improved city walkability and more disabled-friendly transportation.
Activities to bring purpose to older adults are addressed both through work opportunities and volunteerism. However, as well as flexible and remote work helping to make this possible, the prevalence of age discrimination is a significant detrimental force that requires a “California for All Ages” media campaign. Within volunteerism, it’s noted as a way to “support and connect adults” and that “older Californians have much to contribute to our society and to younger generations of Californians, therefore, developing opportunities for multi-generational exchanges is critical.” While not made explicit, this kind of exchange would in itself reduce ageism. To monitor these activities, the state is collecting data on the “Percent of adults age 60 or older who reported having done volunteer work or community service in the past year that they had not been paid for”.